The Relationship Between Dead Space Fraction and End-Tidal Carbon Dioxide
Introduction
In the assessment and management of the respiratory system, dead space fraction (VD/VT) and end-tidal carbon dioxide (ETCO₂) are two crucial indicators. Their correlation is not only extensively studied in medical research but also forms a critical basis for diagnosing and treating respiratory diseases in clinical practice. This article aims to introduce the basic concepts of these two indicators, discuss their relationship, and highlight their importance in clinical applications.
What is Dead Space Fraction (VD/VT)?
Dead space fraction refers to the proportion of gas in a breath that does not participate in gas exchange. Tidal volume (VT) is the total amount of gas inhaled or exhaled during each breath, while dead space (VD) includes anatomical dead space and physiological dead space. Anatomical dead space refers to the conducting airways from the nose to the bronchi, whereas physiological dead space refers to parts of the lung where gas exchange does not occur effectively despite reaching the alveoli.
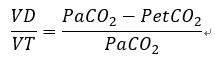
The commonly used method to measure dead space fraction is the Bohr equation, which calculates it by comparing the arterial carbon dioxide partial pressure (PaCO₂) with the end-tidal carbon dioxide partial pressure (PetCO₂):
What is End-Tidal Carbon Dioxide (ETCO₂)?
End-tidal carbon dioxide refers to the concentration of carbon dioxide measured at the end of expiration. It is an important indicator for assessing alveolar ventilation efficiency and overall gas exchange. ETCO₂ measurement is typically performed using capnography devices, providing real-time insights into a patient's respiratory status.

Relationship Between VD/VT and ETCO₂
There is a close relationship between dead space fraction and ETCO₂:
1. Gas Exchange Efficiency:
Ideally, all inhaled air should participate in gas exchange, resulting in ETCO₂ concentration close to arterial carbon dioxide partial pressure (PaCO₂). However, an increase in dead space reduces the amount of air participating in gas exchange, leading to a decrease in ETCO₂ concentration.
2. Disease States:
Certain respiratory diseases such as chronic obstructive pulmonary disease (COPD) and emphysema increase physiological dead space, thereby decreasing ETCO₂ concentration. Monitoring ETCO₂ can indirectly assess changes in dead space fraction and the severity of lung diseases.
3. Ventilation/Perfusion Ratio (V/Q Ratio):
In ideal conditions, the ratio of ventilation to perfusion should be balanced. An increase in dead space disrupts the V/Q ratio, affecting end-tidal carbon dioxide concentration. Monitoring ETCO₂ helps evaluate V/Q imbalance and infer changes in dead space.
Normal Range and Abnormal Conditions
In healthy adults, the dead space fraction (VD/VT) typically ranges from 0.20 to 0.35. This means that approximately 20% to 35% of each breath's tidal volume does not participate in gas exchange.
High Dead Space Fraction:
When the dead space fraction exceeds 0.35, it may indicate respiratory dysfunction or pathological conditions such as:
Chronic Obstructive Pulmonary Disease (COPD)**: Increased dead space fraction and decreased ETCO₂ concentration.
Emphysema**: Structural damage to alveoli reduces gas exchange area, increasing dead space.
Acute Respiratory Distress Syndrome (ARDS)**: Elevated dead space fraction indicates severe lung injury and impaired gas exchange.
Pulmonary Embolism (PE)**: Reduced blood flow to parts of the lung increases physiological dead space, leading to decreased ETCO₂ concentration.
Low Dead Space Fraction:
A dead space fraction below 0.20 is uncommon but may occur in specific situations such as hyperventilation, where end-tidal carbon dioxide concentration may be higher.
Clinical Applications
1. Assessment of Lung Function:
In healthy conditions, the dead space fraction in adults ranges from 0.20 to 0.35. An increase in dead space fraction suggests pulmonary dysfunction, necessitating further evaluation and treatment.
2. Diagnosis and Management of Diseases:
Monitoring dead space fraction and ETCO₂ is valuable in various respiratory diseases:
Chronic Obstructive Pulmonary Disease (COPD): Increased dead space fraction and decreased ETCO₂ concentration. Monitoring ETCO₂ helps assess disease severity.
Pulmonary Embolism (PE): Reduced blood flow increases physiological dead space, decreasing ETCO₂ concentration.
Acute Respiratory Distress Syndrome (ARDS): Elevated dead space fraction indicates severe lung injury and impaired gas exchange.
3. Anesthesia and Mechanical Ventilation Monitoring:
During anesthesia and mechanical ventilation, monitoring VD/VT helps adjust ventilation parameters for effective gas exchange. ETCO₂ monitoring aids in evaluating ventilation status and depth of anesthesia.

Dead space fraction and end-tidal carbon dioxide are critical indicators for assessing respiratory function. By understanding and monitoring these parameters, healthcare providers can better evaluate respiratory efficiency, diagnose and manage respiratory diseases, and optimize respiratory therapy plans. This is crucial for improving patients' respiratory function and overall health. Through this article, we hope to provide clearer insights into the relationship between dead space fraction and ETCO₂.
